WATCH AND LEARN
Share with:
CHICKENPOX: THE BASICS

Welcome to Chickenpox Aware, your go-to resource for understanding chickenpox (or varicella, as it’s scientifically known!). This highly contagious disease is caused by the varicella zoster (VZ) virus.1 While it’s easily spread, the good news is that once your child has had chickenpox, they typically won’t catch it again.2
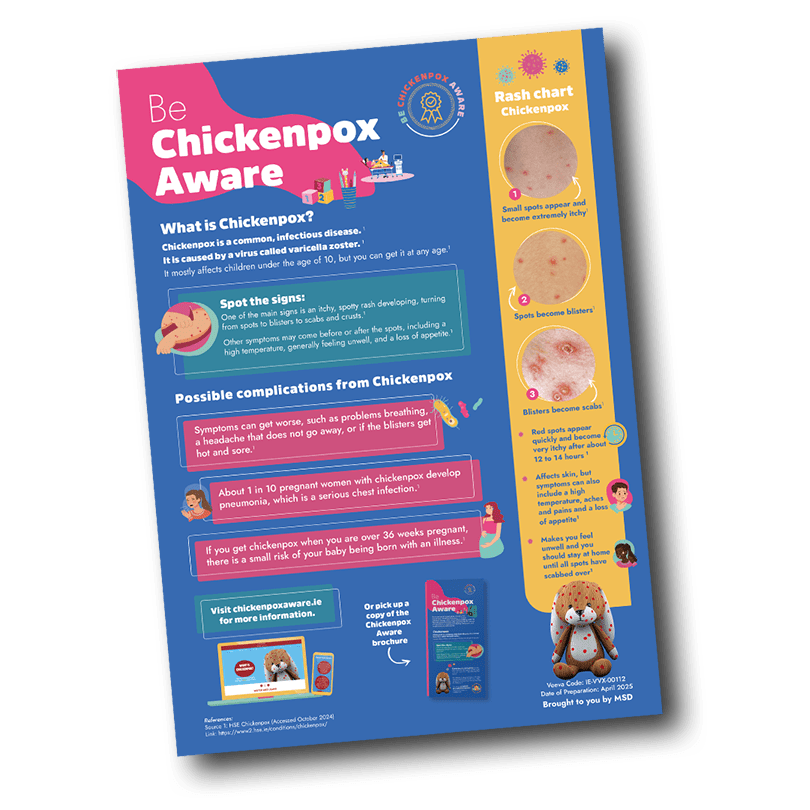
SPOTTING CHICKENPOX / SYMPTOMS
Identifying chickenpox can be tricky, especially since other illnesses can cause rashes. Keep an eye out for these early signs in your little one:

Initial Symptoms: The illness often begins with fever, aches, and an overall sense of feeling out of sorts for about 2 to 3 days.3

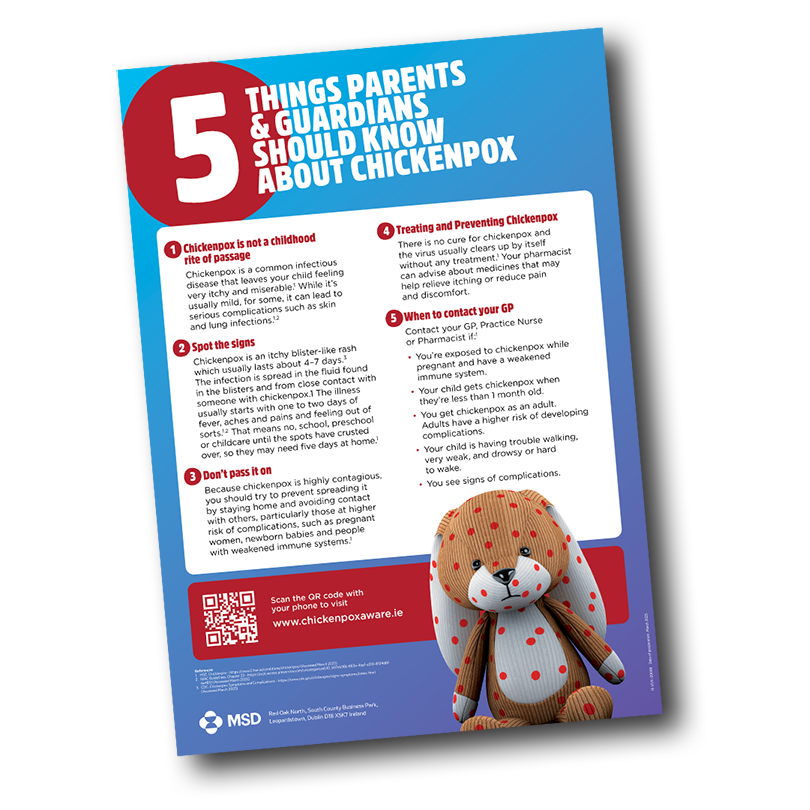
The Rash: Soon after, an itchy rash appears, transforming from small spots to blisters, and eventually scabs.2 The number of spots can vary—some kids are barely affected, while others may have rashes that cover most of their body.3

Contagion Risk: Remember, chickenpox is contagious and can be spread through the fluid from blisters and droplets from coughs or sneezes.2
Your child can be contagious from 2 days before the rash appears until all the blisters have crusted over, which generally takes about 5 to 7 days.2
DON’T PASS IT ON!
To protect others, especially those at higher risk like pregnant women and individuals with weakened immune systems, please keep your child away from school, preschool, or childcare until their spots have crusted over.2


Be prepared for about five days at home to care for them, so you might need to adjust your work schedule.2

If you’re planning to fly, check with the airline, as they may require the last blister to have scabbed over. If the rash is still present, a doctor’s note might be needed.2
HIGH RISK GROUPS
Chickenpox can occasionally lead to serious complications, particularly for adults, pregnant women, newborns, and individuals with weakened immune systems.2
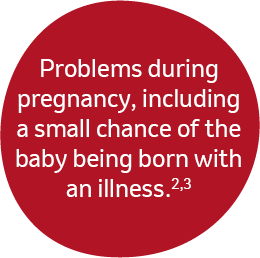
Pregnant Women
If a pregnant woman contracts chickenpox, there is a small risk that her baby could be born with a related condition, especially if she gets it later in her pregnancy (after 36 weeks).2
Post-Exposure Prophylaxis
If you or someone you know falls into a high-risk category and has had significant exposure to chickenpox, it’s crucial to seek immediate medical advice.3
POSSIBLE COMPLICATIONS

If you develop infections, you may need to contact a healthcare professional.2

There may not always be signs of chickenpox complications. However, you should look out for hot or painful skin, difficulty breathing or dehydration.2
If you see any possible signs of complications, contact your GP, Practice Nurse or Pharmacist immediately.2
If you have had chickenpox, you have a greater risk of developing shingles in later life. This can happen when the immune system is low and the chickenpox virus becomes reactivated. Though they are both caused by the same virus, chickenpox and shingles are different diseases.2
WHEN TO CONTACT YOUR GP
Chickenpox is usually mild and clears up in about a week. However, some people can become seriously ill and need to see a doctor.2

Contact your GP, Practice Nurse or Pharmacist if:2
- You think you have chickenpox.
- You get chickenpox as an adult. Adults have a higher risk of developing complications.
- You’re exposed to chickenpox while you’re pregnant.
- You think your child has chickenpox and they are under 1 month old.
- You’re exposed to chickenpox and have a weakened immune system.
- The skin around the chickenpox blisters is hot and sore.
- If your child is having trouble walking, very weak, and drowsy or hard to wake.
TREATING AND PREVENTING CHICKENPOX
There is no cure for chickenpox and the virus usually clears up by itself without any treatment.2
Paracetamol is the preferred painkiller for treating the associated symptoms of chickenpox.2
This is due to a small risk of non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or aspirin, causing adverse skin reactions during chickenpox.2,4
Never give your child aspirin if you suspect or know that they have chickenpox.2
Consult Your Pharmacist
They can recommend treatments to relieve itching or pain.2
Avoid Scratching
This can lead to infections or scarring.
Keep your child’s nails short and consider using gloves or socks at night.2

Stay Hydrated
Encourage fluid intake to prevent dehydration.
Ice lollies can be a tasty and soothing way to keep your child hydrated, especially if they have spots in their mouth.2

Consult your doctor
If complications develop from chickenpox, it is crucial to consult your doctor,
who will determine the appropriate course of treatment.
When booking a doctor’s appointment, make sure to inform the receptionist that your child has chickenpox.
This information is vital, as you may need to arrange a special appointment to minimize the risk of infecting other patients in the waiting area.2
Need more information on chickenpox?
Talk to your doctor, nurse, or pharmacist about chickenpox today

Help spread awareness, not chickenpox!
Download and share our informative guides to keep your loved ones and other parents informed and prepared.
Resources

Links
- NHS – https://www.nhsinform.scot/illnesses-and-conditions/infections-and-poisoning/chickenpox – Accessed June 2025
- HSE – https://www2.hse.ie/conditions/chickenpox/ – Accessed June 2025
- NIAC Guidelines. Chapter 23 – https://rcpi.access.preservica.com/uncategorized/IO_b07eb36b-663e-4ba1-a310-8104d8fda480/ – Accessed June 2025
- CDC. How to Treat Chickenpox – https://www.cdc.gov/chickenpox/treatment/index.html – Accessed June 2025